Autoimmune Disease in Women
 The Facts
The Facts
Named a major women’s health issue by the Office of Research on Women’s Health at the National Institutes of Health (NIH), autoimmunity is the underlying cause of more than 100 serious, chronic illnesses. OF the 50 million Americans living and coping with autoimmune disease (AD), more than 75 percent of them are women.
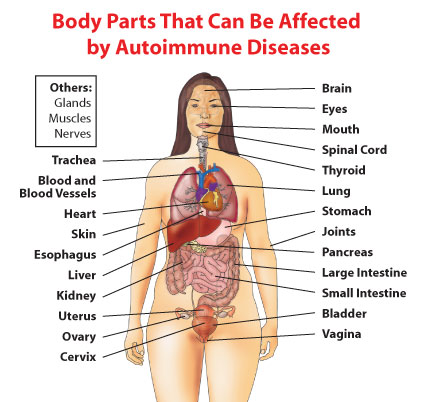
The term “autoimmune disease” refers to a varied group of illnesses that involve almost every human organ system. It includes diseases of the nervous, gastrointestinal, and endocrine systems, as well as skin and other connective tissues, eyes, blood and blood vessels. In all of these ADs, the underlying problem is “autoimmunity” – the body’s immune system becomes misdirected and attacks the very organs it was designed to protect.
Autoimmunity is a Disease Category
Unlike cancer, which is an umbrella category for a range of diseases (leukemia, breast cancer, prostate cancer, non-Hodgkin’s lymphoma, et al.), autoimmunity has yet to be embraced by the medical community (and the public) as a category of disease. Because these diseases cross the different medical specialties, such as rheumatology, endocrinology, hematology, neurology, cardiology, gastroenterology, and dermatology, and because such specialties usually focus on singular diseases within their particular category, there has been virtually no general focus on autoimmunity as the underlying cause. It has been estimated that ADs are responsible for more that $100 billion in direct health care costs annually.Autoimmunity and Women
Taken together, autoimmune diseases strike women three times more than men. Some diseases have an even higher incidence in women. Autoimmune diseases have been cited in the top ten leading causes of all deaths among U.S. women age 65 and younger.1 Moreover, these diseases represent the fourth largest cause of disability among women in the United States.2The fact that women have enhanced immune systems compared to men increases women’s resistance to many types of infection, but also makes them more susceptible to ADs.
In addition, women who have an autoimmune disease have suffered from a lack of focus and a scattered research approach. For example, autoimmunity is known to have a genetic basis and tends to cluster in families as different autoimmune diseases — a mother may have lupus; her daughter, juvenile diabetes and Hashimoto’s thyroiditis; her sister, Graves’ disease; and her grandmother, rheumatoid arthritis.
Different ethnic groups are more susceptible to certain autoimmune diseases. In lupus, for example, African-American, Hispanic, Asian and Native American women are two to three times more likely to develop the disease than Caucasian women.3 And 9 out of 10 people who have lupus are women.4
In 2013, two epidemiological studies published in the online edition of the journal, Arthritis and Rheumatism, confirmed this long-held belief by the American Autoimmune Related Diseases Association, Inc. (AARDA) and many others in the autoimmune disease community – that Systemic Lupus Erythematosus (SLE or lupus) disproportionately affects young African-American women. However , these studies revealed the incidence rate is far greater and impacts these women at a much earlier age than previously thought.
The two studies from National Lupus Registries in Georgia and Michigan are from the largest and most far-reaching epidemiology study ever conducted on lupus. An extensive review of records from hospitals, specialists’ offices and clinical laboratories within Georgia and Michigan showed African-American females developed lupus at a younger age than white females.
Getting an Autoimmune Disease Diagnosis
Since the women affected are mostly young women in their childbearing years, a time when they are traditionally most healthy, getting a diagnosis can prove to be extremely difficult. Symptoms vary widely, notably from one illness to another and even within the same disease. And because the diseases affect multiple body systems, their symptoms are often misleading, which hinders accurate diagnosis.According to a survey by the Autoimmune Diseases Association, over 45 percent of patients with autoimmune diseases have been labeled chronic complainers in the earliest stages of their illness. In addition, another AARDA survey found that it takes most autoimmune patients up to 4.6 years and nearly 5 doctors before receiving a proper autoimmune disease diagnosis.
Despite these statistics, autoimmune diseases remain among the most poorly understood and poorly recognized of any category of illness. Individual diseases range from the benign to the severe. To help women live longer and healthier lives, a better understanding of these diseases is needed, as well as better, more effective methods of diagnosis and treatment.
What Can Be Done?
As the nation’s only organization dedicated to bringing a national focus to autoimmunity as a category of disease and a major women’s health issue, AARDA is working hard on several fronts to raise awareness, including:1. Recognizing autoimmunity as a “category” of disease. If the public and medical practitioners were more aware of the genetic predisposition to develop autoimmune disease, clearly there would be more emphasis on taking a medical history regarding autoimmune diseases within the family when presented by a patient with confusing symptoms. Young women, especially, are often not taken seriously when they first begin consulting their ndoctors for their vague symptoms and are often shunted from specialist to specialist.
2. Increasing public education about autoimmunity and autoimmune disease. Every five years, AARDA conducts a national public opinion poll gauging Americans awareness of AD. The latest survey (2013) indicates greater awareness is still sorely needed. The good news is that over the last decade, Americans’ ability to name and AD has jumped by nearly 10 percent. The bad news, though, is that overall less than one in five Americans — or 15 percent — can name an AD.
3. Creating Autoimmune Diagnostic Triage Clinics or Autoimmune Centers of Excellence. These types of centers are one of the best answers to the critical need for early diagnosis which may prevent significant and lifelong health problems. These clinics would allow patients, whose symptoms are confounding their own physician, to see various medical specialists at one time, rather than going from doctor to doctor over the course of months or years.
4. Facilitating more collaboration and cross fertilization of basic autoimmune research. Research that focuses on the etiology of all autoimmune related diseases will bring us to the root causes of these diseases rather than the superficial level of treating the symptoms after the disease has had its destructive effects.
1. Walsh, SJ, LM. Autoimmune Diseases: A Leading Cause of Death among Young and Middle-Aged Women in the United States. American Journal of Public Health. 2000;90:1463-1465
2. U.S. Department of Health and Human Services. Office on Women’s Health. Women’s Health Issues: An Overview. Fact sheet. May 2000.
3. Society for Women’s Health Research and the National Women’s Health Resource Center, Inc. Autoimmune Diseases in Women.2002.
4. National Women’s Health Information Center. U.S. Department of Health and Human Services, Office on Women’s Health. WomensHealth.gov/faq/lupus.pdf
source: http://www.aarda.org/autoimmune-information/autoimmune-disease-in-women/

